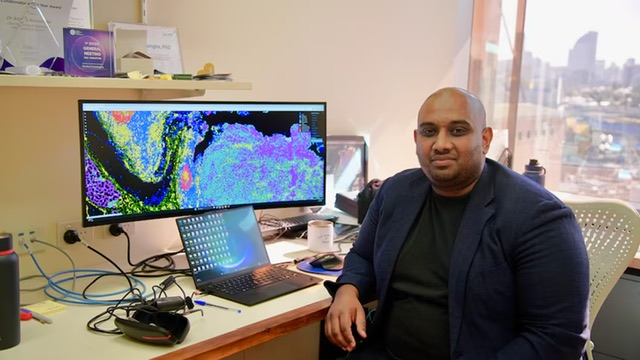
University of Queensland scientist Associate Professor Arutha Kulasinghe, a researcher of Sri Lankan origin, has led a global study that could transform how lung cancer patients are treated.
The research, published in Nature Genetics, has uncovered a way to predict whether patients with non-small cell lung cancer will respond to costly immunotherapy drugs such as Keytruda, which work for only about 20 to 30 per cent of patients.
Kulasinghe and his team analysed lung tumour biopsies from nearly 250 patients across Australia, the United States, and Europe, using advanced microscopes and artificial intelligence to map millions of cells in each sample.
Their findings revealed a “molecular fingerprint” — a pattern showing how immune and tumour cells interact — that can indicate whether a patient is likely to benefit from immunotherapy. “Certain immune cells are in close proximity to tumour cells in patients that do well on immunotherapy,” Kulasinghe explained. “Those patterns are really important to screen for.”
The discovery could allow doctors to test patients before prescribing treatments that can cost up to half a million dollars a year and sometimes cause severe side effects. It may also pave the way for new combination therapies to boost patient response.
Lung Foundation Australia CEO Mark Brooke hailed the study as “an incredible breakthrough,” saying it brings new hope for patients worldwide.
For Kulasinghe, whose passion for cancer research began as a child watching his grandfather battle the disease, the goal is clear: “To make sure every patient gets the right treatment at the right time.”
